We have seen a glimpse of the future of health care during the pandemic this past year. Tools such as telemedicine and video platforms were quickly deployed to provide care to patients with chronic disease at their own homes in order to keep them from overwhelming hospital systems that have channeled all their resources to take care of the critically ill COVID-19 patients.
For providers to care for patients with chronic diseases across the continuum, there is a great need to collect and evaluate patient generated health data (PGHD), whether from remote patient’s devices or other sources, in real time.
Adoption of Digital health Transformation will have a more far-reaching effect on healthcare of the future. It will not only improve quality of care, but also will increase access to affordable care.
For the digital transformation to live up to its promise and potential, a model for delivering accessible and affordable quality care must be developed. An inter-professional model that is based on collaboration and the use of tools and process could facilitate digital transformation now and the future.
Remote Patient Monitoring (RPM)
Researchers from the Appalachian College of Pharmacy have designed an inter-professional model for Remote Patients Monitoring for pharmacists that could be used by other professionals such as nurses, doctors and other healthcare providers. A pilot project was conducted over the past two years to test the pharmacist model in rural southwest Virginia in collaboration with the Carilion clinic pharmacy department.
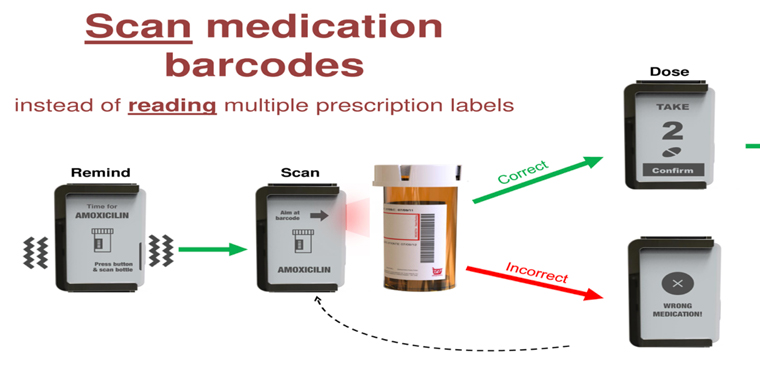
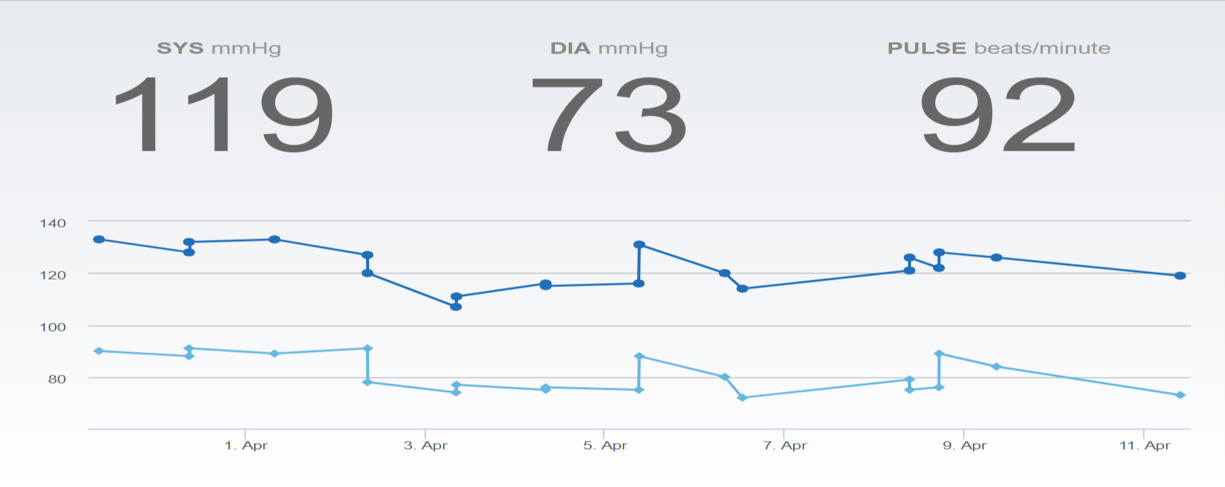
The model utilizes vendors to mail remote monitoring devices directly to the patient home upon the order of the provider. Devices include blood pressure monitors, pulse oximeters, glucose meters and scales and other devices that transmit data to a cloud portal via cellular, Bluetooth or Wi-Fi technology. A Pharmacist, a nurse or a clinical staff, or the provider, will use the portal to monitor the patient transmitted data under the general supervision of the provider. The pharmacist model has an added advantage of providing medication therapy management (MTM) and chronic care management (CCM) to improve patient satisfaction and outcomes.
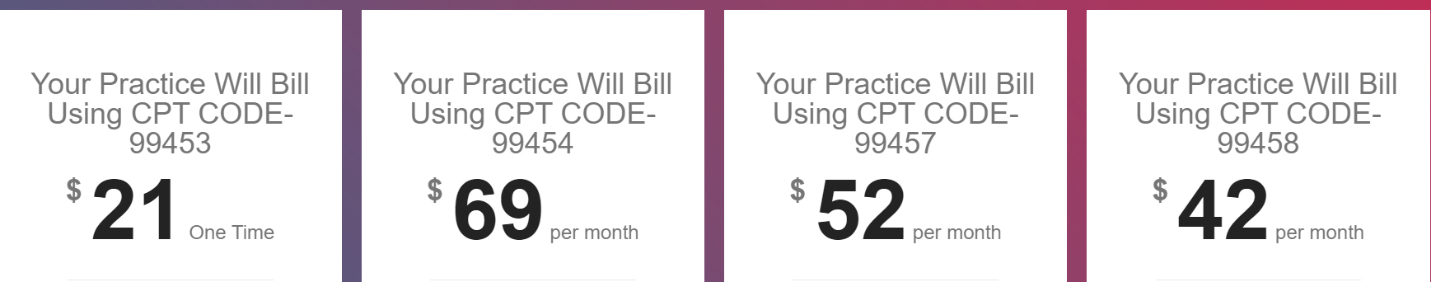
Providers using the program for their patients can reduce clinical burnout and generate a new revenue stream for their practices up to $1000 per patient per year, as explained below.
Hospital and health systems can use the program to augment their Transition of Care (TOC) efforts and reduce hospital re-admission and can achieve great cost savings, which is particularly important to Accountable Care Organizations.
Then the provider can bill for the services utilizing CMS approved CPT codes for Remote Patient Monitoring (RPM).
Digital Health and Remote Patient Monitoring Workgroup
The researchers also have formed a Virginia statewide digital health and remote patient monitoring (DHRPM) workgroup. The role of the Workgroup is to provide a platform for sharing collective experiences and expertise in the area of digital health and to educate and disseminate best practices in digital health by providing educational seminars and webinars.
The researchers also established a digital health and remote patient monitoring call and support center in Roanoke, Virginia, to be a resource for any entity interested in digital health transformation.

Membership is free and open to all individuals, stakeholders, Academia, organizations (Private and public), associations and vendors.
Goals of the Workgroup:
- Advocating the use of virtual care tools for at home monitoring by leveraging telemedicine and remote patient monitoring to shift the center of care from the hospital to the home
- Supporting efforts of improving patient and provider engagement virtually
- Encouraging efforts to expand and design new care delivery of the future, such as digital health, remote patient monitoring, virtual care and telemedicine visits models
- Advancing and integrating digital health tools in everyday care by collecting patient data outside of the clinic or the hospital and making it available for care coordination and chronic disease management to improve health outcomes by using Telehealth and Remote Patient Monitoring (RPM) to improve care and cost savings
- Fostering the adoption of telehealth and remote patient monitoring by multidisciplinary teams that include pharmacists to provide Medication Therapy Management (MTM), Transition of Care (TOC), disease management and patient education and expanding the use of telehealth in chronic diseases such as diabetes, cardiovascular, cancer and substance use disorders (SUD) and others
To learn more about the program or to join the workgroup, please contact Shamly Abdelfattah, PharmD, Associate Professor of Pharmacy Practice Appalachian College of Pharmacy: Phone:1(276)608-8093, email: sabdelfattah@acp.edu

